Continuous glucose monitoring is an alternative to self-monitored blood glucose testing (SMBG); the traditional finger stick tests which take a measurement of blood glucose levels to help patients monitor and manage their diabetes.
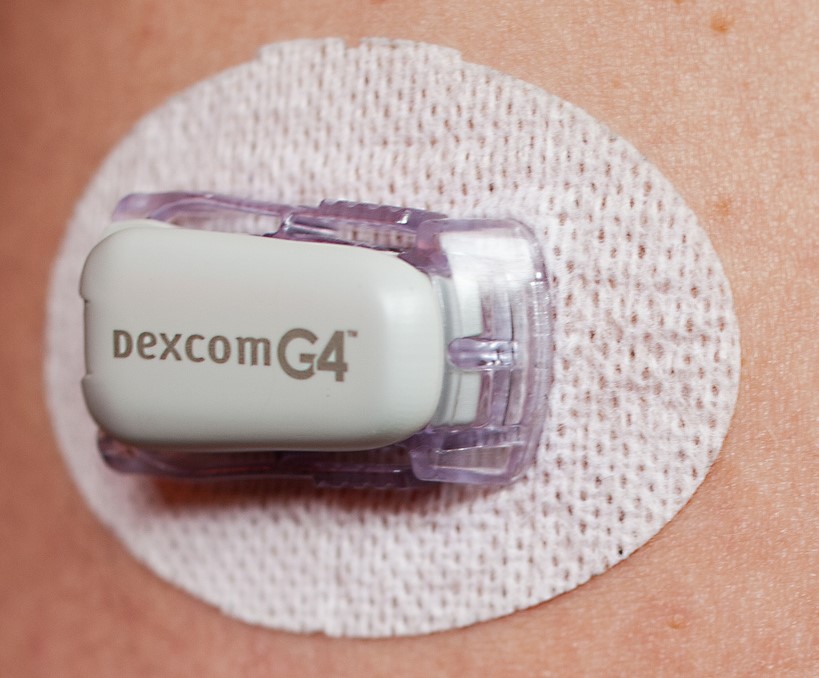
With CGM, patients have a small sensor placed under the skin on their abdomen, which takes a glucose reading every five minutes and sends the data back to a receiver – giving 288 measurements every 24 hours. The receiver is about the size of a pager and can be attached to the patient’s belt; or, in the most recent models, an app on the patient’s iPhone or Apple Watch can act as the receiver.
In this article you’ll find out how CGM is benefiting diabetes patients, and how it can now be used to deliver clinical trials that are simultaneously smaller and more powerful than ever before. Some of the benefits include:
- Collect 288 blood glucose level readings every 24 hours, as opposed to the typical 6-8 readings you might get from SMBG testing.
- Access a wealth of data that also provides the context to understand exactly how your trial drug is affecting patients’ health.
- Drastically improve patient compliance and reduce attrition from trials by making the process much easier for patients.
- Reduce data loss and human error by automatically collecting data through a digital receiver.