These initially consumer facing innovations have opened a world of opportunities for the pharmaceutical industry.
In fact, projections for the global wearable healthcare market suggest significant growth. Forecasts indicate the market will be worth $139.4bn in 2026, having grown from $24.6bn in 2018 (2). In this article, we discuss the range of current and future benefits – as well as the challenges – regarding the application of wearable devices in clinical trials.
Consumer healthcare wearables
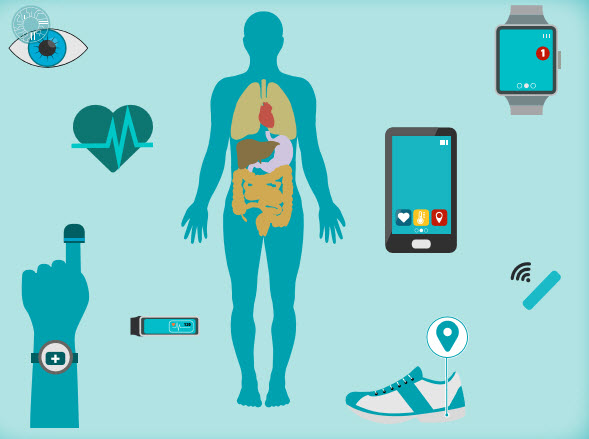
Consumer healthcare wearables include smart phone apps, chest straps, sports watches and other monitoring sensors that can be worn on the body; like the FitBit range of products and Withings ScanWatch, with ECG and SpO2 sensor. These products track users’ physical activity using smartphone and GPS technology.
ResearchKit, launched by Apple, provides an open-source software framework allowing researchers to create apps that can collect clinical data via wearable devices and smartphones.
The integration of wearable health monitors with smartphones now offers increasing capabilities to collect and store health data in real time. As long as a person is operating the device, data can be collected continuously to provide larger samples, and samples that give a fuller picture of a person’s health and performance – as opposed to a snapshot in time that lacks the context of what happened before and after.
In a research setting, this has the potential to provide data to researchers faster, and to improve accuracy in record keeping because it does not rely on a person manually recording data. Additionally, there may be the potential to improve patient recruitment for trials by using technology that minimises the requirements on patients to manually collect data or to make clinical trial site visits.
Increased use of wearables in clinical trials
An increasing number of pharmaceutical and biotechnology sponsors are already using wearables to realise the potential benefits. Around 1,400 clinical trials have been conducted using wearable devices (3)
These studies involve therapeutic areas including asthma, cancer, schizophrenia and diabetes. Just a couple of examples include:
Rheumatoid Arthritis Analysis
GlaxoSmithKline used Apple ResearchKit in a study for rheumatoid arthritis called PARADE, which was supported by an iPhone app. This was the first time that a pharmaceutical company had used the open source software framework to conduct clinical research (4).
Quality-of-Life Tracking
The US Memorial Sloan Kettering Cancer Center (MSK) teamed up with cloud-based analytics company Medidata to assess myeloma patients’ quality of life. These study patients will use wearables to continuously track their activity and sleep, and mobile apps to answer surveys about life quality aspects such as appetite and fatigue. If this pilot study proves accurate, reliable and easy for patients to use, then MSK researchers are planning to expand this research to a larger trial. Medidata may also plan to partner with other organisations if the MSK study goes well (5).
Benefits for clinical researchers
When used in single blinded trials, biometric data collected from medical healthcare wearable devices in clinical trials can potentially offer researchers several qualitative and practical benefits including:
- A real-world view of a patient’s response to treatment by providing a view of their ongoing health status and response to the trial drug that is more objective than the patient recording their experience anecdotally
- Earlier decision-making by providing access to near continuous real-time data. For example, researchers may make amendments to protocols based on how participants are reacting to a drug, and data from wearable technology could contribute to the decision making process.
- More accurate intervention triggers by alerting researchers to potential adverse events or patient non-compliance sooner during the trial.
- An improvement in subject retention by delivering prompts, encouraging compliance and sharing information to encourage active patient participation.
- Reduced costs by decreasing the time and expense of clinic visits. As well as opening up the potential for different approaches to research, analysing data from mobile sensors can provide researchers with extra information to help show the benefits of a drug, to supplement existing research methods.
Challenges of mHealth in clinical trials
There are clearly a range of benefits regarding the use of wearables in clinical healthcare research, however, there are still several questions to be answered (6).
For example, security and privacy − what is the risk of private patient data being accessed by the public? Another issue focuses on data accuracy and validation of data − has the patient worn the wearable device at all relevant times during the trial without tampering or hindrance? There are also ethical issues around the data, such as gaining approval and ownership of the information generated. Finally, there is the challenge of effectively implementing mHealth technology on a global scale.
Improving the experience for patients
In addition to offering benefits for clinical researchers, wearable medical devices can also provide patient benefits. Wearables allow data to be collected digitally and automatically – so patients may not need to keep manual data records. They may also be under less pressure to recall this information in a detailed manner during clinical trials.
Using wearable health devices may reduce the need for clinical visits, giving participants a greater degree of independence, which may in turn increase the likelihood that patients will or can enrol in a trial.
Fortunately, pharmaceutical companies and clinical research organisations do not need to face these challenges alone. Working with expert supply chain partners for the procurement and distribution of quality clinical wearables can help achieve clinical trial success for researchers and patients, on a local and global scale.
Summary
Wearable healthcare devices are already providing a valuable tool to use in conjunction with more traditional methods of research by offering results in an improved context. For example, they may allow researchers to analyse and personalise treatment for specific patient groups. In addition, the use of wearable medical devices in clinical trials can also offer patients a more consistent and convenient experience and encourage patient enrolment and participation in future trials.
References
- Niklas Morton, David Blackman. The Growing Availability of Wearable Devices: A Perspective on Current Applications in Clinical Trials. May 2016. http://www.appliedclinicaltrialsonline.com/growing-availability-wearable-devices-perspective-current-applications-clinical-trials Accessed Nov 2016.
- Fortune Business Insights Wearable Medical Devices Market 2020
- Global Industry Size, Growth, Segments, Revenue, Manufacturers and 2026 Forecast Research Report Accessed March 2020 clinicaltrials.gov – clinical
- Kris Barker. Getting personal with wearable tech. http://www.pmlive.com/pmhub/market_access/adelphi_research_uk/white_papers_and_ resources/getting_personal_with_wearable_tech Accessed Nov 2016.
- Donald Power. Wearables Prove Research Chops in U.S. Cancer Study. https://www.digitalthirst.com/item/wearables-prove-research-chopsin-u-s-cancer-study Accessed Nov 2016.
- S. Food and Drug Administration. Draft Guidance for Industry: Intent to Exempt Certain Class II and Class I reserved Medical Devices from Premarket Notification Requirements. August 2014 http://www.fda.gov/ucm/groups/fdagov-public/@fdagov-meddev-gen/documents/ document/ucm407292.pdf Accessed Nov 2016.